Although some ASR hips have failed, and some may fail in the future, most of the patients I have seen (over 90%) are doing very well at this time. The important point is that patients with an ASR hip replacement should make a follow-up appointment with their orthopedic surgeon, so he or she can check you and your device, and follow your progress over time.
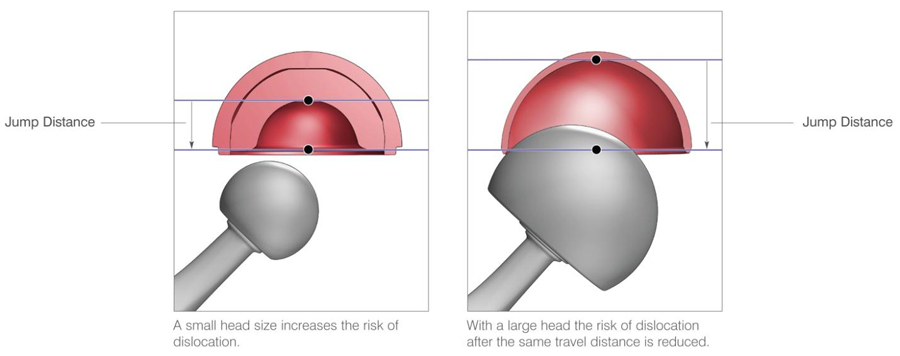
 You may have seen some commercials on TV telling you to check on the status of your hip replacement. This is because Johnson & Johnson’s Depuy orthopedic unit took a dramatic step when they announced a “product recall” on one particular hip implant called the ASR system. While 93,000 ASRs were implanted worldwide, the number in the United States is much less. Some were performed here in Arizona. Most of these hips are still doing very well and meeting patient’s expectations for a successful hip replacement. Although some ASR hips have failed, and some may fail in the future, most of the patients I have seen (over 90%) appear to be doing very well at this time. The important point is that patients with an ASR make a follow-up appointment with their orthopedic surgeon, so he can check you and your device, and follow your progress over time. We are able to check your cobalt and chromium levels by ordering a simple blood test. (Most turn out to be normal!). If the hip becomes “progressively” painful, or you develop a new limp you didn’t have before, that is a warning sign, and you should come in to be seen by the orthopedic surgeon. There are other diagnostic tests we can do, such as Bone scan, metal artifact reduction MRI, ultrasound, and comparison x-rays over time. Interestingly, in the 90 percent of patients that I have seen that are still doing well, they are doing extraordinarily well, meaning the original promise of a more stable hip ( the bigger head makes it harder to dislocate), and the hope that elimination of plastic parts that may eventually wear out, leading to a later preventable revision, have been real benefits.
You may have seen some commercials on TV telling you to check on the status of your hip replacement. This is because Johnson & Johnson’s Depuy orthopedic unit took a dramatic step when they announced a “product recall” on one particular hip implant called the ASR system. While 93,000 ASRs were implanted worldwide, the number in the United States is much less. Some were performed here in Arizona. Most of these hips are still doing very well and meeting patient’s expectations for a successful hip replacement. Although some ASR hips have failed, and some may fail in the future, most of the patients I have seen (over 90%) appear to be doing very well at this time. The important point is that patients with an ASR make a follow-up appointment with their orthopedic surgeon, so he can check you and your device, and follow your progress over time. We are able to check your cobalt and chromium levels by ordering a simple blood test. (Most turn out to be normal!). If the hip becomes “progressively” painful, or you develop a new limp you didn’t have before, that is a warning sign, and you should come in to be seen by the orthopedic surgeon. There are other diagnostic tests we can do, such as Bone scan, metal artifact reduction MRI, ultrasound, and comparison x-rays over time. Interestingly, in the 90 percent of patients that I have seen that are still doing well, they are doing extraordinarily well, meaning the original promise of a more stable hip ( the bigger head makes it harder to dislocate), and the hope that elimination of plastic parts that may eventually wear out, leading to a later preventable revision, have been real benefits.
Frequently Asked Questions About the ASR Hip Implant Recall
 Q: How do I know if I have an ASR total hip?
Q: How do I know if I have an ASR total hip?
A: Most patients do not know which brand of hip replacement they have. Fortunately, the ASR hips were done in a small minority of all hip replacement patients in Arizona. You must contact your orthopedic surgeon, and he can tell you which brand of hip you have. Other Johnson & Johnson/Depuy hip products are doing very well and have not been recalled. We have NOT seen problems with the Pinnacle version of the metal on metal devise, but we do recommend that all patients with metal on metal hips come in for routine follow up every two years, or if they develop painful symptoms.
Q: How will you know if there is a problem?
A: The overwhelming symptom of a failing total hip is increasing pain over time in the groin area. However, groin and hip pain can be caused by other problems, like hip bursitis, tendonitis, or it can be referred from other areas like the spine. It is mostly “obvious” when one of these hips fails. Most patients I have seen that required revision surgery came into the office with a walker or crutches because the pain had become so advanced. The most difficult group to diagnose have a separate and unrelated problem of trochanteric bursitis – a soft tissue inflammation of the bursa on the side of the hip. That pain is not usually related to failure of the hip implant, and can be treated with physical therapy and cortisone injections.
Q: How urgent is it for me to come in if I am not having pain?
A: It is not urgent. However, you should make a routine follow-up appointment with your orthopedist whenever you can to check up on things. An X-ray and Physical Exam will be done. If you have a well functioning ASR implant, you should probably come in every two years or so to check your cobal and chrome blood levels and get an Xray to see how the bone is reacting (or not reacting) to the metal implants.
Q:Why did my surgeon choose the ASR hip for me?
A: I can answer this question for myself. There were many advantages in the ASR design for certain patients. The large HEAD made it very stable and less likely to dislocate. This helped patients with complex anatomy and higher risk for dislocation recover normal activities faster with less restrictions. It was especially useful for larger patients, heavier patients, and patients with scoliosis (crooked spine). Also the metal on metal design in theory could have led to a “longer lasting hip”, as wearing out of more common plastic liners over time had its own set of long term problems. Interestingly, now that we have had longer follow-up, I have see long lasting excellent results of the ASR in the majority of my patients with the devise!
 Q: Will I need surgery to remove the ASR hip I have?
Q: Will I need surgery to remove the ASR hip I have?
A: For a minority – maybe. But only for those that have significant pain from a failed implant, or possibly for a high level of measured cobalt or chrome in the blood system.
Q: Why would you check the cobalt and chrome levels in my blood?
A: Not every patient requires this blood test. However if you are having hip pain, or are just curious in seeing what your blood levels are, we can order this test for you. It turns out that in a small minority of patients, tiny metal particles may be shed by the friction of the metal on metal components. These can be measured in the blood stream.
Q: Do elevated blood levels of Cobalt and Chrome cause illness.?
A: We are not sure what elevated levels of these metal ions may do over time. There is NO evidence that they cause cancer. Elevated levels of Cobalt in particular in some people can cause fatigue, weakness, or headaches. In some people, the metal ions cause a local reaction of fluid formation and hip inflammation. If the hip inflammation grows over time, it can start to damage normal muscles. Most patients with this level of problem have already been revised.
 Q:Why are these ASR hips failing in higher numbers than other hip systems?
Q:Why are these ASR hips failing in higher numbers than other hip systems?
A: There may be more than one reason. The ASR cup is put in the acetabulum without screw fixation because screw heads would interfere with the smooth metal on metal bearing surfaces. Without screws to hold the relatively shallow cup in place, some people develop a loose cup which can be painful. This is a different mode of failure than from the more concerning metal on metal debris inflammatory mode of failure.
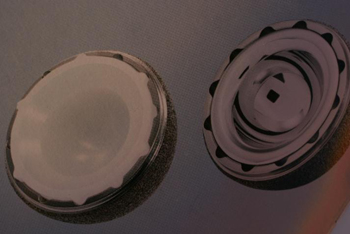
Some cups simply become loose over time because bone fails to grow into them. Other modular hip systems allow for additional fixation when needed by putting screws through the metal shell before a liner is placed (see figure below). Some ASR hips fail because of metal on metal friction and production of inflammatory metal particles in susceptible patients. It is not known why some patients react more seriously to metal particles than other patients.
 Q: What other tests can be done to check on the status of my hip?
Q: What other tests can be done to check on the status of my hip?
A: Other tests your surgeon might order include a bone scan, which is a test that will “light up” in any area where unusual bone turnover is occurring. An special “metal reduction” MRI can be done to look for fluid accumulation around the hip. Likewise, an ultrasound study can be done to detect fluid. Hip aspiration with testing of the fluid can sometimes detect a metal particle reaction. None of these tests are definitive however, and you and your surgeon will decide
together what the next steps should be.
Q: Is revision hip surgery successful?
A: In most cases, I believe that it is. No one wants to have an additional surgery, particularly if the hip is functioning well. But if an ASR failure does occur, a qualified hip surgeon can revise it.
Q: Where can I get more information on this topic?
A: The Johnson& Johnson/ Depuy website has a wealth of useful information. I encourage all patients with questions to visit www.depuy.com and click on the ASR recall button, or the tab that says “patient information”.